Veni project: Reducing health inequalities by opening up E-Health access for digitally non-skilled people.
A Veni Grant is a funding instrument from there NWO talent program. This grant offers your research is the opportunity to you develop their research idea over a period of three years. Esther Metting received this Grant so that she can perform research in the field of eHealtj accessibility of patients with chronic obstructive pulmonary disease (COPD).
Background
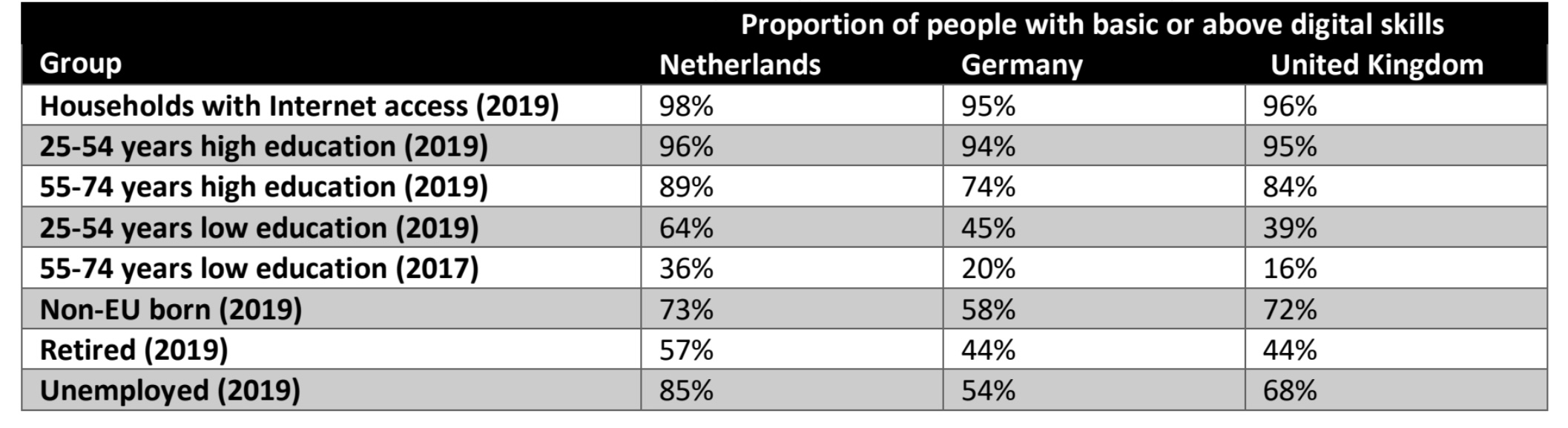
Policy makers including the European Commission consider E-Health (use of technology in healthcare) an important healthcare priority (1) and healthcare providers are increasingly using E-Health in the diagnosis and treatment of patients. This leads to better health outcomes, particularly because care can be tailored to individuals. Unfortunately, Digitally Illiterate People (DIPs) are missing out (2) and have therefore reduced access to optimal healthcare. EHealth can improve health especially in chronic patients (3,4) because symptoms vary over the day and medical assessments are always a snapshot of reality. This complicates clinical decision-making and stresses the relevance and opportunities of E-Health. There are different type of E-Health including tele-monitoring, self-management apps, online disease information or video-conversations. COVID-19 increased the gap between digital literate people and DIPs due to an acceleration of E-Health use (5–9). Access to healthcare is a human right (10) and it is therefore urgently needed to find solutions for DIPs. Digital illiteracy is not the same as health illiteracy: people with good health literacy can still have poor digital literacy (11). The proportion of DIPs is high in older populations (>65 years), in lower educated people and in ethnic minorities even in countries where most household are connected to Internet (table 1). Chronic diseases are also
common in older and lower educated people (12), hence this group can benefit most from E-Health but are in general less capable to use it due to the high proportion of DIPs.
Tailored and theory based decision support methods can help professionals to engage DIPs but are currently not existing (14,15) because DIPs are often not included in intervention studies. There therefore insufficient knowledge about DIPs’ barriers and facilitators (15). Moreover, most E-Health studies were performed in the USA and results are not necessarily generalizable to Europe (14). I have performed qualitative and quantitative (pilot) studies regarding E-Health access for DIPs (16–18). These studies showed that some DIPs were able to use E-Health because they found solutions to overcome their poor
digital skills, for example by engaging digital skilled family members. DIPs mentioned various barriers and facilitators of E-Health that can be divided into: contextual factors (e.g. social support), communicative experience (e.g. ability communicate with healthcare provider), individual factors (e.g. disease), system factors (e.g. app) or interaction between user and technology (e.g. poor vision) (19,20). It is essential to get in contact with DIPs to find tailored solutions to engage them in E-Health and reduce the increasing gap between digital literate people and DIPs.
Theoretical background
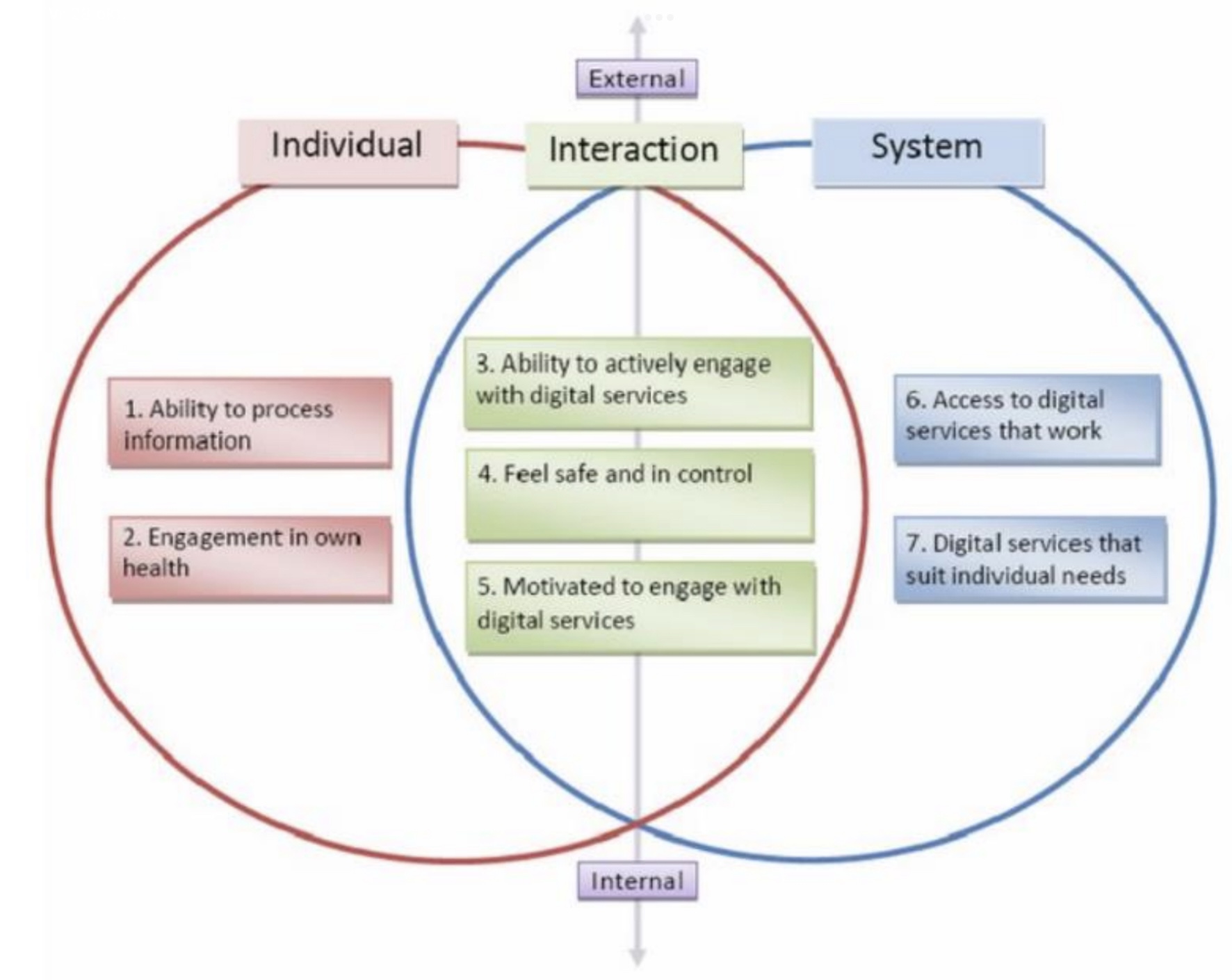
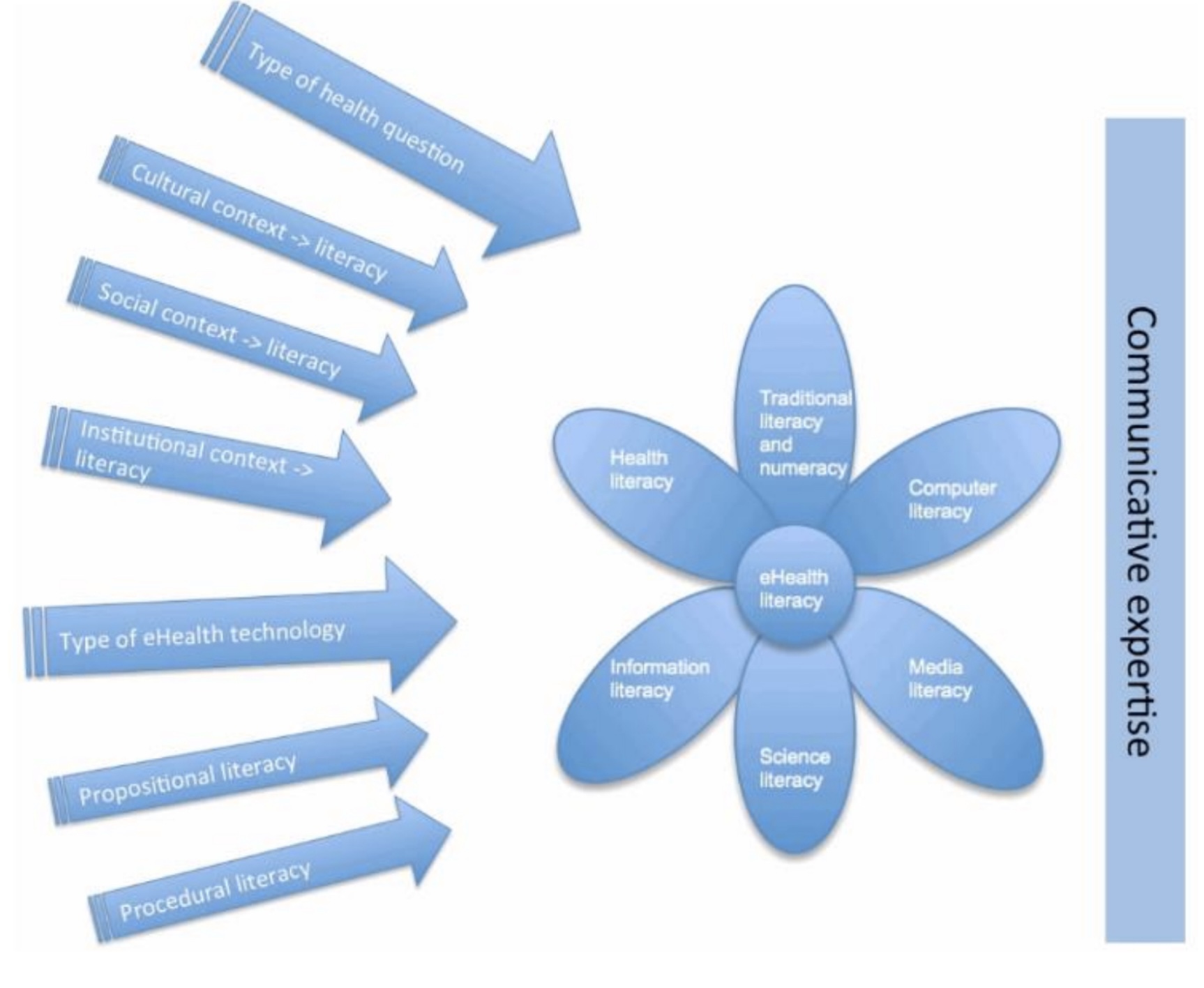
Theoretical concepts can be used in decision support methods and interventions (15). The most leading theories are the “Lily model” (21)), “E-Health Literacy Model” (ELM, figure 1 (21)) and “E-Health Literacy Framework” (ELF, figure 2 (19). The Lily model provides an overview of different types of literacy (see flower in figure 1). ELF consists of 7 E-Health literacy domains divided in 3 dimensions (figure 2). In the E-Health Literacy Model (ELM, figure 1 (21)) contextual and communicative experience are added to the Lily model. The E-Health Literacy Questionnaire (eHLQ) measures the 7 domains from the ELF (19).
In my study I will combine the 7 domains of the ELF (eHLQ) with the contextual and communicational concepts from the ELM to develop a decision support method for healthcare professionals to engage DIPs in E-Health.
Aim of my study
My innovative approach in this Veni project is that I will discover how interactions between factors derived from single factor models (figure 1,2) are related to E-Health. In cocreation with DIPs and healthcare professionals I will develop strategies for different clusters of DIPs, which is unique because DIPs are mostly not included in studies. This is challenging, however my network and experience make this approach feasible. The final aim is to develop a decision support method for healthcare professionals that will enable DIPs to benefit from E-Health References (klein en helemaal onderaan pagina?)
References
1. Communication on enabling the digital transformation of health and care in the Digital Single Market; empowering citizens and building a healthier society | Shaping Euro e’ digital future [ nternet]. [cited 2021 May 7].
2. Sanders CK, Scanlon E. The Digital Divide Is a Human Rights Issue: Advancing Social Inclusion Through Social Work Advocacy. Journal of human rights and social work. 2021 Mar;1–14.
3. RJ J, JQ L, RL O, Caballero J, Jacobs RJ, Lou JQ, et al. A systematic review of eHealth interventions to improve health literacy. Health informatics journal TA – TT -. 2016 Jun;22(2):81–98.
4. (WHO) WHO. Atlas of eHealth country profiles: the use of eHealth in support of universal ehealth coverage. Vol. W 26.5. 2016.
5. Martins Van Jaarsveld G. The Effects of COVID-19 Among the Elderly Population: A Case for Closing the Digital Divide. Frontiers in psychiatry. 020;11:577427.
6. Hassell LA, Peterson J, Pantanowitz L. Pushed Across the Digital Divide: COVID-19 Accelerated Pathology Training onto a New Digital Learning Curve. Academic pathology. 2021;8:2374289521994240.
7. Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME, et al. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic: Bridging or Opening the Digital Divide? Vol. 142, Circulation. United States; 2020. p. 510–2.
8. Lai J, Widmar NO. Revisiting the Digital Divide in the COVID-19 Era. Applied economic perspectives and policy. 2020 Oct; 9. Buchholz BA, DeHart J, Moorman G. Digital Citizenship During a Global Pandemic: Moving Beyond Digital Literacy. Journal of adole cent & adult literacy : a journal from the International Reading Association. 2020;64(1):11–7.
10. Declaration of Alma Ata. The Alabama Journal of Medical Sciences. 1983 Apr;20(2):152–3.
11. Monkman H, Kushniruk AW, Barnett J, Borycki EM, Greiner LE, Sheets D. Are Health Literacy and eHealth Literacy the Same or Different? Studies in health technology and informatics. 2017;245:178–82.
12. Davies JM, Sleeman KE, Leniz J, Wilson R, Higginson IJ, Verne J, et al. Socioeconomic position and use of healthcare in the last year of life: A systematic review and meta-analysis. PLoS medicine [Internet]. 2019 Apr 23;16(4):e1002782–e1002782.
13. Eurostat – internet activities [Internet]. 2019 [cited 2020 Nov 19].
14. Parker S, Prince A, Thomas L, Song H, Milosevic D, Harris MF. Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: a systematic review and realist synthesis. BMJ open. 2018 Aug;8(8):e019192.
15. Watkins I, Xie B. eHealth literacy interventions for older adults: a systematic review of the literature. Journal of medical Internet research [Internet]. 2014 Nov 10;16(11):e225–e225.
16. Metting EI, Verhallen L, de Jong C. Barriers and facilitators of developing and implementing eHealth applications: a questionnaire study with eHealth professionals. European Respiratory Journal [Internet]. 2019 Sep 28;54(suppl 63):PA2239.
17. Metting E, Schrage AJ, Kocks JW, Sanderman R, van der Molen T. Assessing the Needs and Perspectives of Patients With Asthma and Chronic Obstructive Pulmonary Disease on Patient Web Portals: Focus Group Study. JMIR formative research. 2018 Nov;2(2):e22.
18. Metting EI, Baron A-J, Chavannes NH, Tran A, van Luenen S, de Jong C. Evaluation of a pharmacy based personal health record by elderly respiratory patients. European Respiratory Journal [Internet]. 2019 Sep 28;54(suppl 63):PA748.
19. Kayser L, Karnoe A, Furstrand D, Batterham R, Christensen KB, Elsworth G, et al. A Multidimensional Tool Based on the eHealth Literacy Framework: Development and Initial Validity Testing of the eHealth Literacy Questionnaire (eHLQ). Journal of medical Internet research. 2018 Feb;20(2):e36.
20. Gilstad H. Toward a Comprehensive Model of eHealth Literacy. In: PAHI. 2014.
21. Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res[Internet]. 2006;8(2):e9.